Liquid biopsy is proving to be the preferred method for early cancer detection due to its quick, minimally invasive procedure and more comprehensive tissue profile as opposed to a standard needle biopsy. The liquid biopsy shows a more complete picture of the tumor genome and provides the ability to monitor tumor evolution during the course of the disease, enabling physicians to test the DNA traces of cancer in the blood, determine the best course of treatment and track treatment success(Gerber et al., 2020). This can mean the difference between life and death for cancer patients as early detection is essential for patients to have the best chance for successful treatment.
A liquid biopsy, also known as a circulating tumor (ct) DNA assay (ctDNA) is a test done on circulating tumor cells or shed fragments of tumor DNA from a sample of blood to determine the genomics or molecular portrait of a tumor (Wei & Gregg, 2022). On the other hand, a percutaneous tissue biopsy, also known as a needle biopsy, is done by inserting a special needle through the skin to collect cells from a suspicious area. For tumors that can’t be accessed with other biopsy procedures, or if other biopsy procedures have had inconclusive results, a surgical biopsy may be necessary. 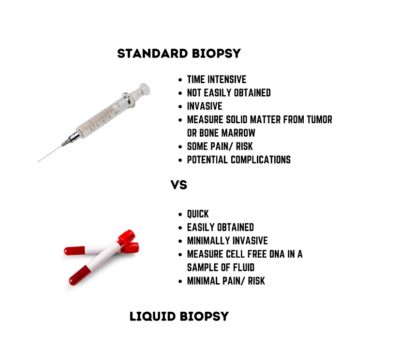
Both approaches are much more invasive than a liquid biopsy, which is collected through a simple blood sample. There are risks to both the patient and the quality of the results with a needle biopsy. First, the patient may experience bleeding, pain and potentially infection, and in very rare cases tumor seeding, which is when the needle inserted into a tumor during a biopsy dislodges and spreads cancer cells (ASCO Staff, 2022).
As for the results, sampling for tumors can be difficult depending on the cancer type and location – there may be an inadequate amount of tissue for genetic testing. According to the Translation Cancer Institute, “In the case of advanced or metastatic non-small cell lung cancers (NSCLC) as many as 31% of cases do not have accessible tissue”. As for the other 69%, preservation methods can cause C > T transitions through deamination of cytosine, potentially leading to false positive results for genetic tests. Due to tumor heterogeneity – the difference between tumors in patients, cancer cells, etc. – biopsies often suffer from sample bias (Brock et al., 2015).
The adoption of liquid biopsy is accelerating, as a recent IASLC statement paper recommends that “liquid biopsy can be considered at the time of initial diagnosis in all patients with advanced NSCLC who need tumor molecular profiling, particularly when tumor tissue is scarce, unavailable, for patients in whom invasive procedures may be risky or contraindicated”, or if the turnaround time for tissue biopsy is anticipated to be longer than two weeks (Wei & Gregg, 2022).
According to Current Pathobiology Reports,
One major barrier [to the more rapid adoption of liquid biopsy] is the lack of standardized pre-analytical workflows, including the collection of consistent quality blood specimens and the generation of good-quality plasma samples therefrom. Broader use of liquid biopsies in clinical routine applications therefore requires improved pre-analytical procedures to enable high-quality specimens to obtain unbiased analyte profiles (DNA, RNA, proteins, etc.) as they are in the patient’s body (Grölz et al., 2018).
To ensure the success of liquid biopsies, a process must be in place to keep the biopsy from contamination through the pre-analytical, transportation and processing phases. Multiple pre-analytical variables including blood sampling, handling, ctDNA extraction procedures, and transportation and storage temperatures may tamper with the quantity and quality of ctDNA. As a result of many clinical trials, plasma is the preferred matrix for liquid biopsy and should be used over serum as it has greater sensitivity (Wei & Gregg, 2022). Plasma is the liquid that remains when clotting is prevented with the addition of an anticoagulant and serum is the liquid that remains after the blood has clotted. Fresh plasma must be stored at −20°C or −80°C for long-term stability of DNA. It has been shown that extracted DNA from blood samples is stable at 4°C for several weeks, at −20°C for months, and at −80°C for years (Grölz et al., 2018).
Keeping a biopsy for months and even years is important for many reasons. First, some patients want a second opinion on the diagnosis made from their tissue sample (specimen). This is called a pathology review. It means getting another doctor to look at the biopsy tissue and make a diagnosis on what’s seen. Human tissue samples are not discarded right after testing. So, in most cases, if there’s enough tissue, the sample can be sent to another doctor or lab.
If a cancer survivor develops a tumor several years after the first one was removed, doctors will want to know if this new tumor is the old one coming back (a recurrence) or a completely new cancer. This can often be done based on the locations of the two tumors and by comparing the histopathology slides from both specimens. But sometimes, more tests (such as immunohistochemical stains) that can be done using tissue from the original specimen’s paraffin block are also helpful.
Finally as techniques evolve newer techniques can be used on previous specimens to gain additional information.
Using an alternative solution to dry ice is advised for transporting samples which aids in the longevity of the sample. Phase change materials (PCMs) maintain low temperatures longer than dry ice depending on which PCM is used, insulation, amount of PCM and environmental temperatures.
Remove the inconvenience, cost, and environmental complication associated with cleaning up, disposing and replenishing dry ice when transporting specimens with a green, sustainable alternative approach that PCMs provide. Learn more about how PCMs can replace the need for dry ice and enable the success of liquid biopsies and cancer detection and treatment.
- Wei, D., & Gregg, J. P. (2022, February 6). A brief introduction to clinical application of liquid biopsy. lab-best-practice. Retrieved November 9, 2022, from https://health.ucdavis.edu/blog/lab-best-practice/a-brief-introduction-to-clinical-application-of-liquid-biopsy/2019/07
- Gerber, T., Taschner-Mandl, S., Saloberger-Sindhöringer, L., Popitsch, N., Heitzer, E., Witt, V., Geyeregger, R., Hutter, C., Schwentner, R., Ambros, I. M., & Ambros, P. F. (2020, June 1). Assessment of pre-analytical sample handling conditions for comprehensive liquid biopsy analysis. The Journal of Molecular Diagnostics. Retrieved November 9, 2022, from https://www.sciencedirect.com/science/article/pii/S1525157820303512
- Grölz, D., Hauch, S., Schlumpberger, M., Guenther, K., Voss, T., Sprenger-Haussels, M., & Oelmüller, U. (2018, October 18). Liquid biopsy preservation solutions for standardized pre-analytical workflows-venous whole blood and plasma. Current pathobiology reports. Retrieved November 9, 2022, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6290703/
- Brock, G., Castellanos-Rizaldos, E., Hu, L., Coticchia, C., & Skog, J. (2015, June 18). Liquid biopsy for cancer screening, patient stratification and monitoring. Translational Cancer Research. Retrieved November 9, 2022, from https://tcr.amegroups.com/article/view/4546/html
- ASCO Staff. (2022, May 16). Can a biopsy make my cancer spread? Can a Biopsy Make My Cancer Spread? Retrieved November 9, 2022, from https://www.cancer.net/blog/2021-03/can-biopsy-make-my-cancer-spread


